Clinical case: Exocrine Pancreatic Insufficiency in a German Shepherd Dog

ANAMNESIS
A 1 year old German Shepherd bitch correctly vaccinated and dewormed is presented in consultation for chronic diarrhea evolving since 3 months, associated with weight loss (4 kg loss during this period) with a normal to increased food intake. A dietary change (hypoallergenic diet) did not lead to improvement. The volume and frequency of bowel movements were increased. Stools are often mucusy. Borborygmas and flatulence are reported.
CLINICAL EXAMINATION
On clinical examination, the dog remains in good general condition despite a body score of 3/9. Abdominal palpation is flexible and painless. The intestines are thickened and we note a liquid and gas dilatation of some handles. The rest of the clinical examination was unremarkable.
DIAGNOSTIC HYPOTHESES
History and clinical examination point us towards diarrhoea of the small intestine with a severe malassimilation syndrome. The main diagnostic hypotheses retained are: parasitic infestation, diarrhoea responding to antibiotic treatment (dysbiosis), chronic inflammatory bowel disease, exocrine pancreatic insufficiency or chronic pancreatitis, cholestatic liver disease or liver failure, endocrine disease (hypoadrenocorticism), digestive neoplasia (lymphoma carcinoma), food intolerance or allergy, renal insufficiency.
FURTHER EXAMS
The coproscopic examination performed on faeces collected over 3 days is negative.
Mild normocytic normocytic anemia (10.4 g/dL, VU = 12.4 - 19.1 g/dL) is present at the hematological examination. On biochemical examination there is a moderate hypoalbuminemia (20 g/L, VU 23-34 g/L). Ionogram (Na K Cl) is normal.
Basal cortisol at 155 nmol/L rules out hypocorticism.
Ultrasound examination of the abdomen is performed. Marked thickening is noted and diffuse of the intestinal wall without loss of echo structure. The adrenals are of sizes normal (6 mm). Moderate to marked diffuse mesenteric adenomegaly is noted.
The remainder of the examination is normal.
Serum Trypsin concentration measured by the Trypsin-Like Immunoreactivity method is low (<2.5 μg / L, VU = 5 to 35 μg/L). Severe undosable hypocobalaminemia is present.
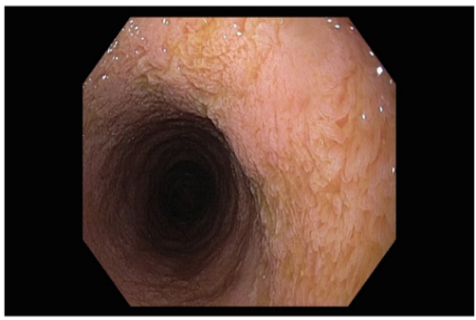
An endoscopic examination is performed because of hypoalbuminemia and the possibility of concomitant bowel disease. The duodenum has increased granularity as does the ileum. The remainder of the examination shows no particular abnormality. Histological analysis reveals discrete lympho-plasmic inflammation with severe crypt hyperplasia consistent with chronic antigenic stimulation.
DIAGNOSIS
The presence of low serum ILT concentrations associated with typical clinical signs of maldigestion are considered diagnostic of exocrine pancreatic insufficiency.
MANAGEMENT
The basic treatment includes supplementation with pancreatic enzyme extracts (in the dog's food at each meal), antibiotic therapy with metronidazole (15 mg/kg morning and evening), and cobalamin supplementation (500 μg in SC once a week for 6 weeks and then once a month). A hyperdigestible food is introduced as a first line of treatment.
EVOLUTION
Clinical follow-up of the dog confirmed rapid clinical improvement with normal stool consistency soon after initiation of treatment. Weight gain was also noted after 1 month.
The prognosis for this dog remains reserved but depends mainly on the response to treatment. Indeed, nearly 20% of dogs with PEI are euthanized within the first year following diagnosis and 17% only partially respond to treatment.
COMMENTS
Exocrine Pancreatic Insufficiency (EPI) is an uncommon condition at the origin of a malassimilation syndrome, the management of which is complex. If the diagnosis and treatment seem simple, the management of affected animals is complex and can lead to nutritional deficiencies. In the presence of signs of maldigestion secondary to CAI, enzyme compensation is indicated. The basic treatment includes supplementation with pancreatic enzyme extracts in the dog's food, at each meal or food intake, even if the food is considered hyperdigestible. Various extracts of pancreatic enzymes are available in France, and the choice is based on practical properties, availability and costs.
An increase in the amount of substrate for bacteria in the small intestine due to maldigestion, the absence of bacteriostatic factors in the pancreatic fluid, and changes in intestinal motility or an associated chronic inflammatory bowel disease are possible causes of bacterial accumulation in the small intestine. Antibiotic therapy with metronidazole (15 mg/kg BID) for periods of 1-3 weeks is often required for animals with CAI. Nevertheless, it should be noted that if the flora is modified by the pancreatic disorder, treatment by adding pancreatic enzymes allows a gradual return to normal flora. Once the treatment with exogenous enzymes and the adapted diet has been implemented, and in particular when the animal resumes of weight, antibiotic therapy should not be prolonged.
However, their use may be useful when clinical signs, such as diarrhea, increased intestinal gas production and flatulence, are not resolved by enzyme therapy, or when these signs have reappeared during long-term treatment. Chronic untreated bacterial overgrowth can cause mucosal damage that is only partially reversible after even prolonged antibiotic treatment. This may partly explain why some animals do not return to normal body weight despite treatment.