Clinical Case: Chronic diarrhea in a Sharpei dog
ANAMNESIS
A 2 year old male sharpei is presented in consultation for intermittent diarrhea for 6 months with progressive worsening during the last 3 weeks. Weight loss is reported but remains moderate. Appetite is increased. Stools are mainly liquid and of increased frequency, however the owner reports episodic attacks of tenesmus with the presence of mucous stools. These attacks are often accompanied by vomiting.
The pet’s owners report no improvement when switching to a hypoallergenic diet for 1 month. An antibiotic treatment associated with a hyperdigestible diet was subsequently implemented following a negative parasite coproscopic analysis and resulted in a transient improvement in diarrhea. A recurrence is indeed reported at the end of the treatment with a worsening of the general condition of the pet. No other medical history is reported. The dog is properly vaccinated and dewormed (fenbendazole 50mg/kg 3 consecutive days 2 weeks before presentation).
CLINICAL INVESTIGATION
At the clinical presentation the dog remains alert and in good general condition. The body score is evaluated at 4/9. Mild dehydration is noted at 5%. The abdomen is supple and not painful, but an aerial and liquid distension of certain digestive coves is noted. A rectal examination confirms the existence of liquid and nauseous stools that are not mucusy. The rest of the clinical examination shows no significant abnormality.
DIAGNOSTIC HYPOTHESES
The general condition of the animal, which is still satisfactory despite a slight weight loss, seems to eliminate the possibility of a systemic disease, a hypothesis that will however have to be verified by examinations. The characteristics and frequency of diarrhoea in this case do not make it possible to define whether it is the consequence of a disease of the small or large intestine, although the loss of weight and the increase in food intake point towards a malassimilation syndrome.
When dealing with a malassimilation syndrome, it is sometimes useful to categorize the primary site of the condition and to recognize additional factors such as disturbances in gastrointestinal motility that may be important in the management of the patient. There are 3 types of malassimilation classified according to the primary site of disease: intraluminal maldigestion (exocrine pancreatic insufficiency, dysbiosis, hepato-biliary disease), mucosal malabsorption (inflammatory or neoplastic bowel infiltration disease), and malassimilation due to post-mucosal (vascular or lymphatic) abnormalities.
FURTHER EXAMS
A CBC, biochemical report and urinalysis revealed no abnormalities and rule out a systemic condition. In particular, an ionogram is without abnormality and a basal cortisol at 155 nmol/L rules out adrenal cortical insufficiency. Normal albuminemia should be noted to rule out exudative processes. Coproscopic examination is negative and previous antiparasitic treatment makes intestinal parasitosis unlikely.
The measurement of serum Trypsin concentration by the Trypsin-Like Immunoreactivity method is the most commonly used method to assess pancreatic exocrine function (VU = 5 to 35 μg/L). In our dog, a normal concentration of 15ng/ml was noted, excluding exocrine pancreatic insufficiency. The diagnosis directs us towards a malabsorption syndrome of intestinal origin. Malassimilation tests showed an abnormal elevation of folate (18 ng/ml, VU = 4-13μg/ml), a lowered cobalaminemia (124 ng/l, VU = 200-400 ng/l). These results are in favour of dysbiosis.
Ultrasound examination of the abdomen shows no significant thickening of the intestinal wall or abnormality of the parietal echostructure of the intestine. Discrete mesenteric adenomaglie is noted but not suspicious. The remainder of the examination shows no significant abnormalities of other abdominal organs.
As the patient has not responded to the various medical and dietary treatments previously undertaken, an endoscopic examination of the small intestine and colon is considered.
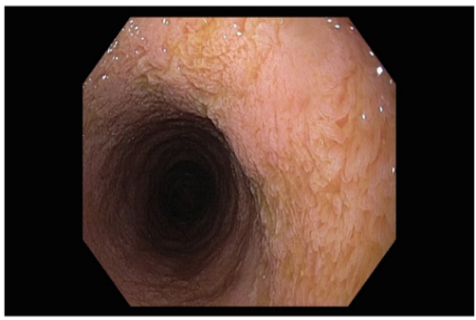
Endoscopic images of the duodenum show no major abnormalities. However, the mucous membrane shows a slightly increased granularity. Note that the duodenal chyme is quantitatively abnormally abundant. Staggered biopsies of the mucosa are taken.
In the colon, the ileal papilla is abnormally incompetent and an examination of the ileum was performed. The mucous membrane is normal in appearance and biopsies were taken.
The mucous membrane of the colon is very congestive. The submucosal vascularization remains clearly visible.
Analysis of the histological samples taken from the proximal small intestine revealed a lymphoplasmocyte-like inflammatory infiltrate invading the villi axis. There is a moderate increase in intraepithelial lymphocytes.
On two duodenal biopsies, the villi are subatrophic. The lymphatic collecting system appears normal. In the ileum, the same type of lesion is reported with more marked villous subatrophy. The colon is normal with just reactive mucoid-like inflammation characterized by caliciform cell hyperplasia.
DIAGNOSIS
This dog shows symptoms, a change in specific biological parameters, histological examination compatible with a chronic inflammatory disease of the lymphoplasmocytic type of moderate grade of the small intestine. Given the age of the animal and its breed, dysbiosis is suspected which may be primary and responsible for the histological lesions observed or secondary to the inflammatory process. Subatrophy of the villi should be considered as a criterion of severity. The malabsorption syndrome in this dog may be secondary to a decrease in absorption surface area (villous atrophy), enterocytic lesions (due to dysbiosis), mucosal infiltration (IBD). Several of these mechanisms may be present concomitantly in this patient. In chronic inflammatory diseases, diet and bacterial antigens play an important role in the etiology of the disease. The mechanisms are speculative, but increased mucosal permeability to antigens and an unregulated immune response appear to be responsible for the disease. Food antigens can induce dysimmune reactions (type I and IV hypersensitivity) and intolerances in the intestinal mucosa.
MANAGEMENT
An antibiotic therapy based on metronidazole (15mg/kg morning and evening) is prescribed for 6 weeks. A hyper-digestible dietary food is prescribed. Vitamin B12 supplementation is introduced (500μg/week for 6 weeks then twice a month) combined with probiotics. Corticotherapy will be considered if the response to antibiotic and dietary treatment is unsatisfactory due to villous subatrophy.
EVOLUTION
The clinical improvement in diarrhea was very rapid, starting in the first week. The animal recovers 8% of its weight after 4 weeks of treatment. Intestinal transit seems to have returned to normal. The owner is warned of the risks of recurrence but of the good prognosis in the long term provided that he keeps a preventive diet.
COMMENTS
If one tries to classify the enteropathy of this dog, the correct response to antibiotics (metronidazole) directs the diagnosis towards an "antibiotic-sensitive enteropathy", which is likely a deviation of the intestinal microfore (quantitative or qualitative) or "dysbiosis". Antibiotic therapy is often necessary and must be prolonged over several weeks (5 to 6 weeks). The antibiotic of choice is metronidazole.

Figure 1 endoscopy: duodenal mucosa.
The villous relief is well preserved but there is villi oedema.

Figure 2 endoscopy: ileal papilla.
There is a certain gap in the papilla which may be responsible for colo-ileal reflux and aggravate dysbiosis.



